Nutrition support management pre and post upper gastrointestinal (GI) surgery | Case Study
Description
The patient is a 68 year old male with a diagnosis of Metastatic adenocarcinoma of the gastric body.
Anthropometry:
Current weight: 68.9kg.
Weight lost: 23kg (25% of body weight in 3 months).
Medical management:
Partial gastrectomy and anastomosis of stomach to jejunum (GI- FOLFIRI) followed by 12 cycles of chemotherapy.
Overall aim/goal:
Maintain weight and achieve a nutritionally complete diet.
Nutritional Requirements:
BMR: 1377 (PAL 1.5)1,2
Protein: 69-83g per day2
Energy: 2065kcal per day2
Fluid: 2070ml2
Dietetic Intervention:
Prior to surgery, the patient was advised on a liquid diet and how to make it nutritionally complete. Blending foods and adding Pro-Cal powder to increase the energy and protein content was explained to the patient. Advice regarding eating little and often and to include small, blended meals was provided. The use of low volume oral nutritional supplements (ONS) such as Pro-Cal shot was also discussed. Post-surgery the aim was the re-introduction of textured foods.
Monitoring/Review:
As part of their management, the patient had monthly dietetic assessments pre surgery where weight, biochemistry (including vitamin D and B12 levels), tolerance of ONS, and bowel habits were all reviewed and managed. After surgery, the patient was followed up in the Upper GI MDT surgical clinic with surgeons, clinical nurse specialists, dietitians, and physiotherapists, to continue their management.
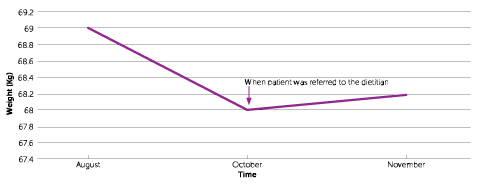
Graph represents patient’s weight over time.
Barriers:
- The patient trialled a number of oral nutritional supplements but experienced taste fatigue with them.
- The patient’s energy levels to prepare and blend meals was low at various time frames which affected dietary intake.
Strengths:
The variety of oral nutritional supplements used (‘compact style’ products along with Pro-Cal shot and Pro-Cal powder), ensured there was always an option available to the patient depending upon their energy levels. A variety of flavours was used to help avoid taste fatigue. Recipe booklets were also provided.
Conclusion:
The patient was able to maintain their weight through guidance and regular follow up from the dietitian. Input from the physiotherapist also ensured the patient maintained their muscle mass.
Key Learnings:
- Finding appropriate oral nutritional supplements that compliment a patient’s lifestyle and symptoms is key to compliance.
- Providing options with oral nutritional supplements in terms of flavour and recipe ideas can increase compliance.
- MDT working is key to maintaining weight, especially muscle mass.
- Henry CJK, Basal metabolic rate studies in humans: measurement and development of new equations. Public health nutrition, 2005, 8 (7a) 1133-1152.
- Department of Health Dietary reference values for food energy and nutrients for the United Kingdom. HMSO, London; 1991.


