
Use of K.Yo as a supplement alongside enteral tube feeding | Case Study
DESCRIPTION
Use of K.Yo as an oral supplementary source of nutrition for a tube fed child with drug resistant epilepsy.
Notes:
K.Yo is a food for special medical purposes and must be used under medical supervision.
Age: 6
Gender: Male
Diagnosis: Sub-acute sclerosing panencephalitis (SSPE)
Relevant family/social history: Lives with mum, dad and older brother
Relevant medical history:
Previously fit and well child, achieving all milestones, nil past medical history until sudden onset of neurological decline with seizures (clonic, tonic-clonic, myoclonic and 1 episode status epilepticus), dystonic posturing, ataxia and cognitive impairment around 5 ½ years old.
Trialled various anti-epileptic drugs (AED's) with no significant improvement in seizure activity; at this point was referred as an inpatient for urgent consideration of ketogenic diet 3 months after his first seizure.
Further investigations including electroencephalogram (EEG), magnetic resonance imaging (MRI) and lumbar punctures showed to have evidence of measles antibodies in cerebral spinal fluid and a subsequent diagnosis of SSPE was made one month after commencing KD.
Medications:
Levetiracetam, gabapentin, clobazam, clonidine, immunoglobulin infusions, ribavarin, melatonin. PRN: buccal midazolam, chloral hydrate, bisacodyl suppositories.
Nutritional history:
Prior to the child’s neurological decline, he ate a wide range of foods, textures and drank fluids. With the progression of disease and onset of seizures, he became less alert (post seizures/side effect of AEDs) and developed an unsafe swallow. A nasogastric tube was placed to meet nutritional requirements and he has since had a gastrostomy tube inserted as a long term route for feeding.
Relevant biochemistry:
Ketogenic blood screen checked prior to starting diet.
Anthropometrics:
On starting KD:
Weight = 20kg (50th-75th centile)
Height = 118cm (75th-91st centile)
Daily estimated energy requirements and ketogenic diet prescription:
| Daily energy requirements | 1480kcal |
| Classic ketogenic diet (CKD) ratio |
Initial ratio 0.5:1 (↑0.5 increment as tolerated) Final ratio 2.5:1 |
| Macronutrients (based on 2.5:1 ratio) |
140g fat 20g protein 36g carbohydrate |
| Micronutrients | RNI for all micronutrients |
| Fluid | 1500ml |
Goals of dietary management:
- Ensure adequate growth and nutritional status; achieve ketosis and reduce seizure activity.
- The parents expectation of management - reduction in seizures, increased alertness and regain some functional skills.
Feed recipe (including 120ml extra volume for priming giving sets):
| Proprietary ketogenic 4:1 liquid feed | 728g |
| Powdered carbohydrate supplement | 38g |
| 50% LCT fat emulsion | 99g |
| Total feed volume | 1120ml (cool boiled water added to make this total volume) |
| Daily bolus plan (89% of total feed volume) | 4x250ml @ 250ml/hr |
| Macronutrients per bolus feed |
35g fat 5g protein 9g carbohydrate |
Speech and language therapy (SALT) assessment:
Shortly after starting the CKD there was a slight improvement in alertness and parents keen to restart oral diet if possible. SALT highlighted that on days when the child is less alert/not managing secretions he should not be offered anything orally. However, on days when the child was more alert and managing secretions he could have a pureed ketogenic diet and sips of water.
Texture modified ketogenic diet:
The parents were given 2.5:1 ketogenic recipes however due to limited availability of texture modified ketogenic foods in hospital and lack of a diet chef this proved quite challenging. K.Yo had the required semi solid texture. It was easy to store when used on ad hoc basis; easily adjusted to obtain required ratio by adding a carbohydrate powder.
K.Yo daily recipe:

| K.Yo | 100g (1 pot) |
| Powdered carbohydrate supplement | 2g |
| Ratio | 2.5:1 |
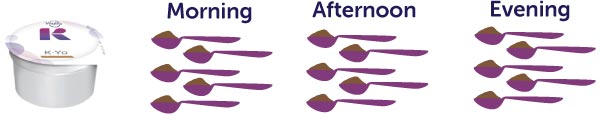
| SALT prescription |
5 level teaspoons x3 times per day |
Education and training:
The CKD was initiated in hospital and the parents were educated on the diet, how to test blood glucose/ketone levels and treat abnormal results. They also received gastrostomy pump training and the milk kitchen staff taught them how to prepare feeds.
Patient progression:
Within 1 week ketones were up to 3mmol/l and he received the first course of immunoglobin infusions and ribavarin started shortly after. During weekly dietetic reviews, no seizures were reported, although it was difficult to attribute seizure freedom to the CKD alone.
Over the following 2 months in hospital, the child remained on the CKD whilst further investigations and treatment were undertaken, and a social care discharge package was arranged. Ketones reduced to approx. 1mmol/l although seizure freedom continued.
Due to the nature of SSPE, there was little improvement in functional skills with variable swallowing capabilities on a daily basis. With the use of K.Yo as a supplementary product this allowed for oral tasters which the patient enjoyed and parents felt involved in food provision.
The patient appeared to really enjoy K.Yo (opened mouth for more) and was able to take the restricted amount prescribed by SALT.
Discharge from hospital:
The child remained on the ketogenic diet for a further 2 months following discharge, continuing to have K.Yo as an oral supplement alongside his enteral feeding regime. At his 3 month follow-up in the keto clinic, his weight had increased to 23kg (75th centile) and height remained static.
After 4 months on the ketogenic diet, the neurological multidisciplinary team agreed to wean him off the diet and monitor any changes to seizure activity. He remained seizure free and subsequently discharged from the dietetic keto team.
From a dietetic perspective it is a very practical product to use in the KD, easy to adjust ratio and take out and about with the child. It is ideal for hospital use, especially if ketogenic catering is limited and for those requiring a texture modified diet.
